
What is treatment for Achilles Tendinopathy?
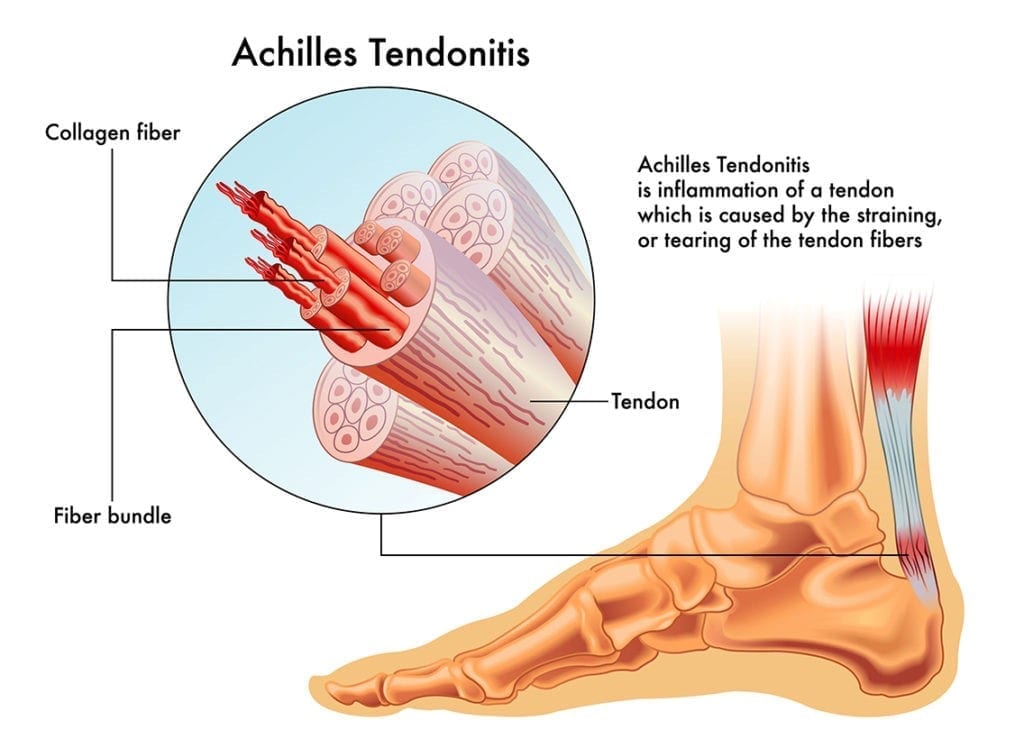
Achilles tendinopathy is a common condition that results in pain in the Achilles tendon, which is the tendon that attaches the calf muscle to the back of the heel bone. Achilles tendinopathy is caused by excess strain or load on the Achilles tendon. This can occur from an acute injury or an overuse (chronic) injury.
Once commonly known as Achilles tendonitis it is now mostly referred to as Achilles tendinopathy because research has found that it is most likely due to tendon fibre micro tears and degeneration rather than inflammation.
Sports that involve repetitive running and jumping are more prone to Achilles tendinopathy and it is estimated that it accounts for 11% of all running injuries.
Signs & Symptoms
The following signs or symptoms may indicate Achilles tendinopathy:
- Pain present in the mid-portion of the Achilles tendon (approximately 5cm from the heel insertion)
- Pain present close to the Achilles tendon’s insertion into the heel
- Stiffness in the tendon especially in the morning or after rest
- Pain can either be present before, after or during activity depending on severity
- There may be associated swelling
- In chronic cases you may feel lumps within the tendon
Causes of Achilles Tendinopathy
Achilles tendinopathy is caused by excess strain on the Achilles tendon. Factors that can increase load and strain on the Achilles tendon include:
- Poor foot mechanics or excess foot pronation
- Tight or weak calf muscles
- Poor ankle joint flexion
- Increase in training or loads
- Inadequate warm up or stretching before sport
- Activities involving running, jumping, hopping or sudden changes of direction
- Poor footwear
Achilles tendinopathy occurs when there is too much strain on the tendon, resulting in small micro tears within the tendon fibers.
Achilles tendinosis occurs when there is repeated micro trauma or degeneration to the tendon. It results in scar tissue build up within the tendon due to the chronic torn fibers. This can often be felt as a lump within the tendon.
Achilles tendon rupture occurs when there is complete or partial tear. This can be the result of an acute incident such as a sudden pivot, jump or acceleration or degeneration of the tendon. An Achilles tendon rupture results in a sharp onset of pain with significant swelling making weight bearing difficult. Athletes may even hear the tendon snap. Surgery if often required for complete Achilles tendon ruptures.
Treatment for Achilles Tendinopathy
- Strapping
- Ultrasound or laser therapy
- Stretching and strengthening
- Footwear advice
- Orthotics
Treatment is firstly aimed at reducing strain on the tendon to reduce symptoms and followed by a focus on progressive exercises to stretch and strengthen the Achilles. Addressing the cause of Achilles tendinopathy is often the key to success and helps prevent a reoccurrence.
Poor foot mechanics and excess foot pronation are often causative factors that get overlooked as this places more strain on the Achilles tendon when the foot rolls in.
Early diagnosis and treatment with a podiatrist can help treat Achilles tendinopathy and prevent it becoming a chronic condition.

What is an Ankle Sprain?
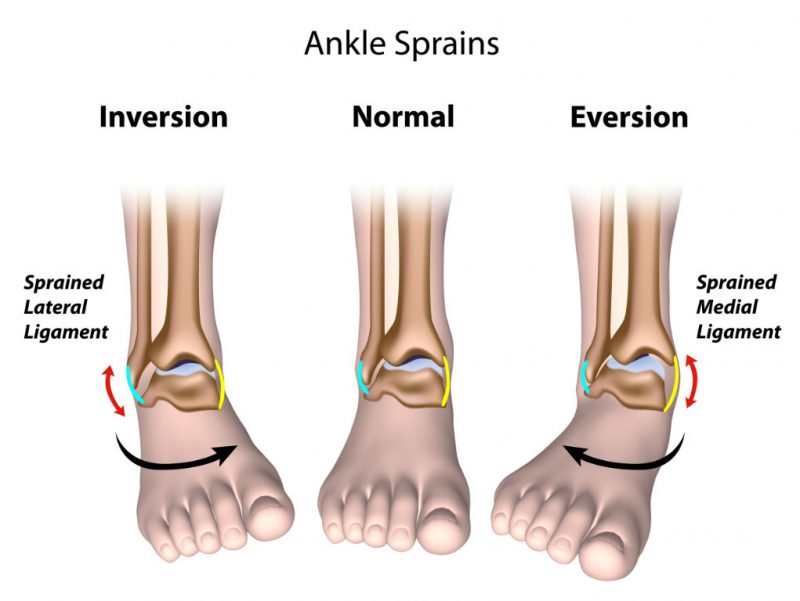
An ankle sprain is an acute injury that causes damage to the ankle ligaments. This results in either a partial or complete tear of the ligaments and leads to pain and swelling around the ankle. Ankle sprains most commonly occur on the outside of the ankle (lateral ankle sprain) but can also occur on the inside of the ankle (medial ankle sprain). If the forces during the acute injury are large then sometimes a bony fracture may result at the ligament attachment site as the ligament tears away from the bone.
Signs & Symptoms
- Swelling around the ankle
- Bruising around the ankle
- Pain or tenderness around the ankle
- Limping or unable to put weight on the affected ankle
- There may be associated ankle instability
- There may be restricted ankle range of motion
Causes of an ankle sprain
Ligaments help stabilise joints and prevent excess joint movement. An ankle sprains occurs when the joint is forced beyond its range of motion causing injury and tears to the ligaments. If the forces during an ankle injury are large then sometimes an associated bony fracture may result at the ligament attachment site as the ligament ruptures from the bone.
Typical causes of a sprained ankle include:
- Twisting or rolling your ankle during a fall
- Twisting or rolling your ankle after landing awkwardly from jumping
- Another person forcefully stepping or landing on your ankle during sport
Ankle sprains most commonly occur to the lateral ankle joint (outside of ankle) and but can also occur to the medial ankle joint (inside of ankle joint). Lateral ankle sprains are usually the result of an inversion sprain (when your ankle rolls out too much), whilst medial ankle sprains are usually the result of an eversion sprain (when your ankle rolls in excessively).
The ankle is one of the most commonly injured body parts during sports. Athletes in sports that involve repetitive jumping and landing (e.g. Australian rules football, basketball, netball) or repetitive side to side movements (e.g. tennis) are more prone to ankle sprains. Athletes with poor foot biomechanics may be more prone to chronic and repetitive ankle sprains. Poor footwear is also a common risk factor in ankle sprains.
Diagnosis
In mild ankle sprain cases further diagnostic studies are usually not required. In more severe ankle sprain cases referral for a x-ray, musculoskeletal ultrasound scan or MRI may be required to diagnose the full extent of the injury and to check for other associated injuries such as fractures and tendon tears. Our podiatrists can refer for these scans without the need for a GP visit.
Treatment for ankle sprains
Treatment options at our clinic for ankle sprains can include:
- CAM Walkers (Moon boots) to help immobilise the ankle
- Strapping
- Ultrasound & laser therapy
- Ankle strengthening
- Ankle braces
- Orthotics
Orthotics help address biomechanical faults and can help make your ankles more stable and less prone to chronic ankle sprains.
If you have suffered from any ankle injury acute or chronic it is important to see one of our podiatrists. Often other problems like fractures get easily overlooked and a podiatrist is best placed at giving you the right rehabilitation for ankle injuries.


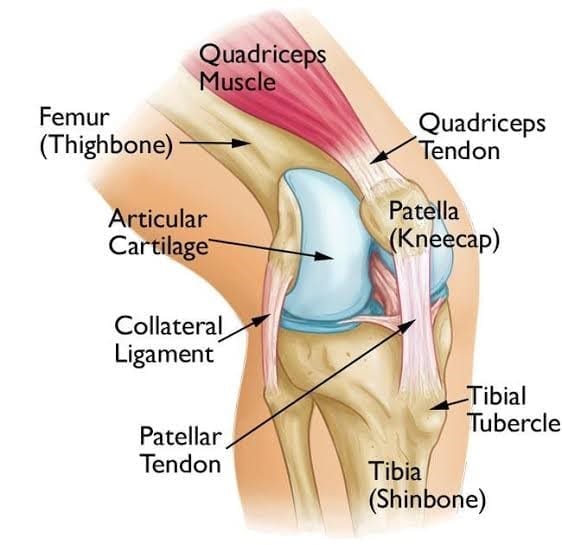
What is Patellofemoral Knee Pain?
Patellofemoral pain syndrome is a condition causing pain behind or around the patella (knee cap) in the knee joint. It is one of the most common causes of knee pain and is also commonly referred to as “runner’s knee” or “jumper’s knee” because it is prevalent in patients who participate in sports. It can however also affect non-athletes and is common in any age group including the young and elderly.
Signs & Symptoms
The following signs or symptoms may indicate patellofemoral pain syndrome:
- Pain present either behind or around the patella (knee cap) in one or both knees.
- Pain may present as a dull ache at the front of the knee during activity.
- Symptoms are often noticed more during activity (especially high impact activity) and relieved with rest.
- Running, jumping, squatting, stairs or activities involving repetitive bending of the knee may exacerbate symptoms.
- In some cases you may hear associated cracking of the knee joint as it bends.
Causes of patellofemoeral knee pain
Patellofemoral knee pain is most commonly caused by poor alignment or tracking of the patella (knee cap) within the knee joint. This causes increased forces or pressure behind the knee leading to irritation of soft tissue and joint surfaces. If left untreated patellofemoral pain syndrome can lead to degeneration of the cartilage behind the patella (knee cap).
Other factors that can cause patellofemoral knee pain include overuse of the patella (knee cap), muscle imbalance or weakness, injury, surgery or poor foot biomechanics.
Poor foot mechanics (e.g. flat feet) are a major cause of patellofemoral knee pain. When your feet excessively pronate or roll in it causes the tibia bone to excessively rotate inwards. This then leads to excess internal rotation at the knee joint and poor tracking of the knee cap resulting in patellofemoral pain. Poor knee alignment can lead to future degeneration or arthritis within the knee joint and chronic pain.
Athletes involved in sports that involve a lot of running or jumping such as athletics, football and basketball may be more prone to patellofemoral knee pain.
Treatment for patellofemoral knee pain
Treatment options at our clinic for patellofemroal knee pain include:
- Stretching and strengthening of muscles
- Footwear advice
- Orthotics
Orthotics work by improving foot function and this helps improve knee alignment. By reducing excess foot pronation (inward rolling of the feet) orthotics can reduce internal tibia rotation, keeping the knee joint straighter during activity.

What is Plantar Fasciitis / Fasiosis?
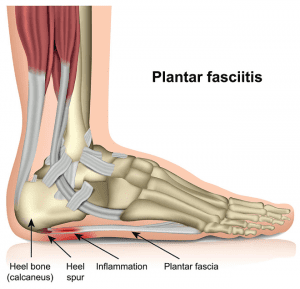
Plantar fasciitis (osis) is a debilitating condition that causes pain in the heel or arch of the foot. It is caused by excessive strain on the plantar fascia ligament on the bottom of the foot.
The plantar fascia ligament is a thick band of fibrous tissue that runs under your arch and attaches the heel to the toes. It supports your arch and helps you walk.
Athletes or runners with poor foot mechanics or feet that excessively pronate (flatten or roll in) are more prone to developing plantar fasciitis as this can place more strain on the ligament. Athletes in sports that involve repetitive running or jumping are also more prone to this condition.
Signs & Symptoms
The following signs or symptoms may indicate plantar fasciitis:
- Pain present on the bottom of the foot in the arch or the heel
- Pain may present as an ache or be a sharp, burning pain
- Pain is usually worse first step in the morning or when you get out of bed
- Pain can also occur standing after being seated for a period
- Pain mostly dissipates on walking but in chronic cases pain may be present on every step
Causes
Plantar fasciitis is caused by excessive strain on the plantar fascia ligament. Factors that can increase load and strain on the plantar fascia include:
• Poor foot mechanics or excess foot pronation
• Excess weight
• Pregnancy due to weight gain and hormonal changes
• Activities involving running, jumping or hopping
• Spending long periods on your feet
• Poor footwear
Plantar fasciitis tends to be more common in the middle aged population, when supporting foot muscles weaken, placing more load on the plantar fascia. It is also slightly more common in women compared to men.
In some cases the resultant ongoing traction of the fascia on the bony attachment can cause bone spurring, commonly referred to as a heel spur.
Athletes involved in sports or activities that place more or repetitive stress on the heel or arch are more prone to plantar fasciitis. This includes sports that involve a lot of running and jumping including football, basketball, athletics, aerobics etc.
Diagnosis
X-rays are not necessary as a heel spur on x-ray makes little difference to the treatment. Interestingly some people with no heel pain can still have a heel spur on x-ray so it is not a useful diagnostic tool. A heel spur simply tells us that there is excessive strain and forces at the ligament attachment site close to the heel bone.
Tarsal tunnel syndrome and other nerve entrapment’s can mimic plantar fasciitis symptoms so our podiatrists will help exclude these from diagnosis. In some instances these conditions may even coexist with plantar fasciitis. For more information please see our page on other causes of heel pain.
Treatment for plantar fasciitis
Our podiatrists have a wealth of experience treating plantar fasciitis and heel pain. It is one of the most common conditions we treat at our clinic and we know what gets results, even in chronic cases. Unlike other therapies, treatment by our podiatrists is aimed at the cause of plantar fasciitis and simply not just reducing symptoms. This treatment strategy helps to prevent plantar fasciitis from returning once it is fully healed. Patients who have had plantar fasciitis for years are often amazed at our success.
Treatment of plantar fasciitis at our clinic may consist of the following:
- Strapping
- Orthotics or arch supports
- Stretching and strengthening exercises
- Footwear advice
Orthotic Therapy
Orthotics can help treat plantar fasciitis as they help support the foots natural arch and reduce strain on the plantar fascia. By doing this orthotics treat the cause of plantar fasciitis. In chronic cases of heel pain our podiatrists find that custom orthotics give better clinical results than prefabricated or “off the shelf” orthotics.
Chronic plantar fasciitis usually affects a high arch foot type with a tight plantar fascia. In this foot type prefabricated orthotics with lower arches simply don’t support the plantar fascia enough. Custom orthotics can be manufactured with a high arch that closely matches the foot and this is why they produce better clinical results in plantar fasciitis treatment. An accurate custom orthotic will support a high arch foot and reduce strain on the plantar fascia. It will also aid in stretching the tight fascia whilst removing forces off the heel insertion area, allowing for healing.




What are Shin Splints?
Shin splints are an overuse injury involving the muscles that attach from the shin bone (tibia) to the foot. It is also commonly referred to as medial tibial stress syndrome or MTSS. Repetitive strain and load on these shin muscles result in muscle fatigue, pain and inflammation at the muscle’s bony attachment site on the tibia.
Signs & Symptoms
The following signs or symptoms may indicate shin splints:
- Pain or tenderness along the inside of of your shin bone.
- Pain may range from mild discomfort to severe burning.
- Pain generally occurs in the middle to lower third of the tibia.
- Symptoms are usually most noticeable at the start of activity or sport and diminish as activity continues.
- Pain can often return following activity or sport and can be worse the next day.
- In severe cases of shin splints or MTSS pain may be continuous.
Causes of shin splints
Shin splints are caused by repetitive strain and load on the shin muscles, resulting in muscle fatigue, pain and inflammation at the muscle’s bony attachment site on the tibia. Risk factors that can increase load on the shin muscles and tibia include:
- An increase in the duration, frequency or intensity of training
- Running on uneven or hard surfaces
- Tight or weak lower leg muscles
- Poor foot mechanics including flat feet and high arched feet
- Poor footwear
Foot biomechanics can play a significant role in shin splints or medial tibial stress syndrome. When you walk or run your feet should ideally pronate (roll in) a little to help adapt to surfaces whilst absorbing shock and forces especially during heel strike. Flat feet or feet that excessively pronate (roll in too much) can cause overuse of the medial shin muscles as they try and slow down this foot movement, resulting in shin splints. High arched feet on the other hand are poor at shock absorption because they don’t pronate or roll in enough. Poor foot shock absorption will transfer the load and forces onto the tibia (shin bone), resulting in shin splints.
Repetitive shin splints can also progress to lower leg stress fractures, as weak shin muscles will transfer the stress onto the bone, which then may result in bone fatigue and a small micro fracture.
Sports that involve repetitive loading like running are often associated with shin splints and they account for approximately 17% of running injuries.
Treatment for shin splints
Treatment options at our clinic may include:
- Strapping
- Stretching and strengthening of lower leg muscles
- Orthotics
- Footwear advice
- Running technique modification
Orthotics can help shin splints by improving foot function and reducing excess foot pronation. In severe cases of shin splints along with some foot types, modification of running technique may be required to successfully reduce forces on the shin bone and resolve symptoms.
What are Stress Fractures?
A stress fracture is a tiny crack or fracture in a bone. Stress fractures are overuse injuries and results from fatigue of surrounding muscles causing failure in the bone. The fatigued muscles are unable to absorb shock and forces and this load is then transferred to the bone leading to failure within the bone, and a tiny crack or fracture.
It is estimated 95% of all stress fractures in athletes occur in the lower legs and feet. In the foot, the most common sites are the metatarsals (especially 2nd and 3rd); whilst in the lower leg it is in the lower third of the tibia and fibula.
Signs & Symptoms
The following signs or symptoms may indicate a stress fracture in the foot or lower leg:
- Pain present in the foot or lower leg that intensifies during activity but relieved with rest.
- Pain is usually gradual in onset and progresses to more focal and intense pain with the onset of swelling.
- Swelling present over the top of the foot or in the lower third of the leg.
- Tenderness at the fracture site.
Causes of a lower leg or foot stress fracture
Stress fractures are caused by overload and overuse, so athletes involved in sports with repetitive stresses like running and jumping are often more prone. Stress fractures are most common in the feet (especially the metatarsals) because there are many small fragile bones within the feet and the feet are responsible for absorbing large forces when walking or running.
Risk factors that can cause lower leg or foot stress fractures include:
- Increase in training load, frequency or duration
- Weakness of lower leg muscles or chronic shin splints
- Running on uneven or hard surfaces
- Diet deficiencies or disease causing a decrease in bone strength
- Poor footwear
- Poor foot or lower leg mechanics
Poor foot mechanics can be a major factor in causing lower leg or foot stress fractures. Unstable flat feet that roll in too much can place more stress and rotation on some of the bones in the feet (especially long fragile bones like metatarsals) which then may lead to bone failure.
Rigid high arched feet are poor at shock absorption and this can send an increase in forces directly to foot and lower leg bones, which may eventually lead to bone failure.
Treatment for lower leg or foot stress fracture
Initial treatment is aimed at removing forces off the fracture site and involves rest to allow for bone healing. Following healing our sports podiatrists can help you with rehabilitation and exercises to help get you back on your feet. Secondary treatment involves identifying and treating the cause of the stress fracture to help prevent a reoccurrence.
Treatment options at our clinic include:
- CAM Walker (Moon Boot) for immobilisation
- Orthotics
- Footwear advice
- Muscle strengthening
They can then prescribe orthotics to help treat lower leg and foot stress fractures. Orthotics can help in a number of ways:
Orthotics with specific padding can help safely offload and stabilise forefoot fractures to allow for bone healing, often without the need for CAM Walkers and crutches.
Orthotics also improve foot function by supporting the arch and reducing excess foot pronation (inward rolling of the feet). This helps address biomechancial causes of stress fractures by making foot bones more stable during loading and propulsion. A more stable foot will also reduce rotation and forces on the lower leg muscles and bones.
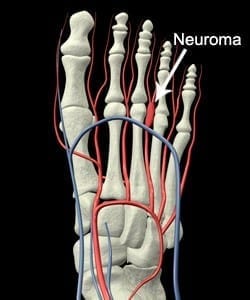
What is Morton’s Neuroma?
A neuroma is a painful condition whereby the nerve passing between the toes becomes entrapped, thickened and irritated. It is most common between the third or fourth toes (known as a Morton’s neuroma), however they can also occur between other toes.
Symptoms
Neuroma symptoms can vary from a mild burning or tingling pain to a sharp shooting pain into the toe. Often a clicking sound is evident when the toes are squeezed together. One theory is that the clicking noise is a bursa (fluid filled sac) that the body develops when two joints rub against each other. This bursa then entraps the nerve causing a sharp radiating pain into the toes.
What causes neuromas?
Neuromas are caused by compression of the toes. This can be caused by previous injuries to the toes leading to instability and compression such as a plantar plate injury. Other causes include wearing shoes that are too tight, poor foot mechanics and excess pronation.
Treatment
Treatment is aimed at stabilising the toes and preventing compression of the toes and nerve. This may involve supportive padding and orthotics to help stabilise the foot and metatarsals. Outcomes are best if treated early by one of our podiatrists. In chronic neuroma cases surgery may be the only effective solution and our podiatrists can help steer you in the right direction.

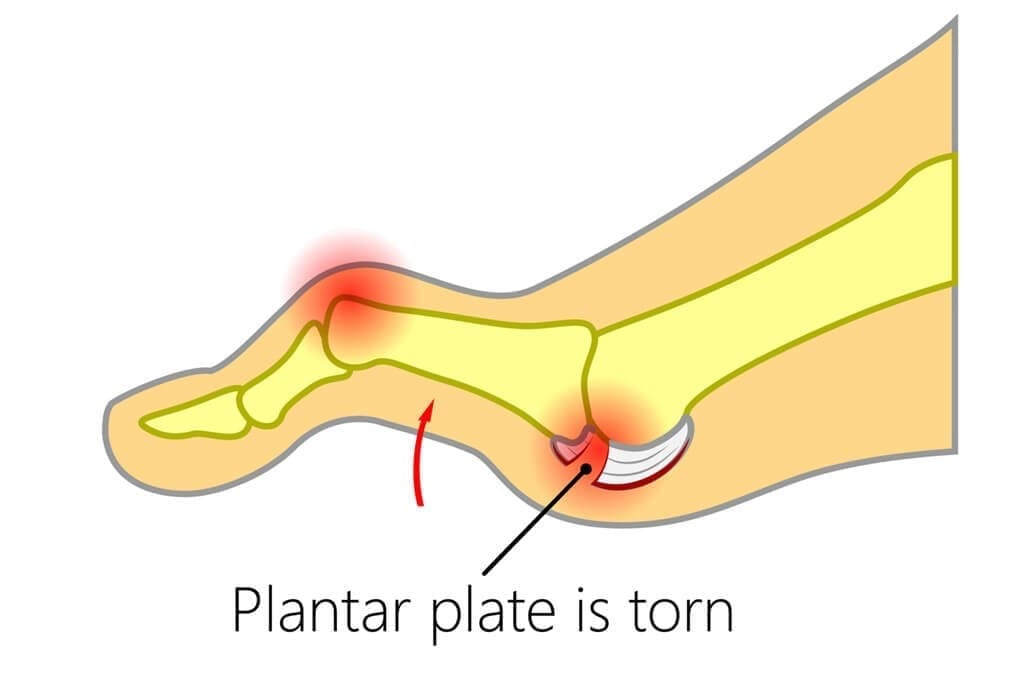
What is a Plantar Plate Tear?
A plantar plate injury is an injury to the thick ligament structure that inserts into the base of the toes or proximal phalanges. The ligament is responsible for stabilising the toe. A tear or rupture to the plantar plate ligament structure results in pain and ultimately an unstable toe. Plantar plate injuries are commonly seen at our Melbourne podiatry clinic, especially in middle aged patients, and it is often a problem that gets misdiagnosed by other health professionals.
Symptoms
Symptoms of a plantar plate injury includes swelling, inflammation and pain on the ball of the foot making walking difficult. A tear of the plantar plate will often result in the toes splaying, whilst a full rupture of the plantar plate will result in toe hyperextension. Symptoms of plantar plate tears and ruptures can often last for months. If the toe remains chronically unstable then this can cause other problems in future like arthritis or neuromas.
Causes
Plantar plate tears and ruptures can be caused by acute or chronic injury to the toe. Acute trauma to the toe such as stubbing the toe can result in a plantar plate injury. They can also occur from chronic overloading forces and excess movement of the toes. Poor foot function or excess pronation can lead to instability of the toes leading to excess pressure on the plantar plate, ultimately resulting in a tear or rupture.
Treatment
Our podiatrists know how to diagnose plantar plate injuries and how to differentiate them from similar foot problems like neuroma and metatarsalgia. Treatment at our clinic focuses on reducing symptoms in the initial phase and this may involve padding and strapping. Once symptoms have settled treatment is aimed at strengthening the joint and stabilising the toe. Our podiatrists can prescribe custom orthotics to help stabilise the foot and toes following a plantar plate injury. Orthotics along with strengthening exercises and good footwear will often be an effective long term management for this problem.

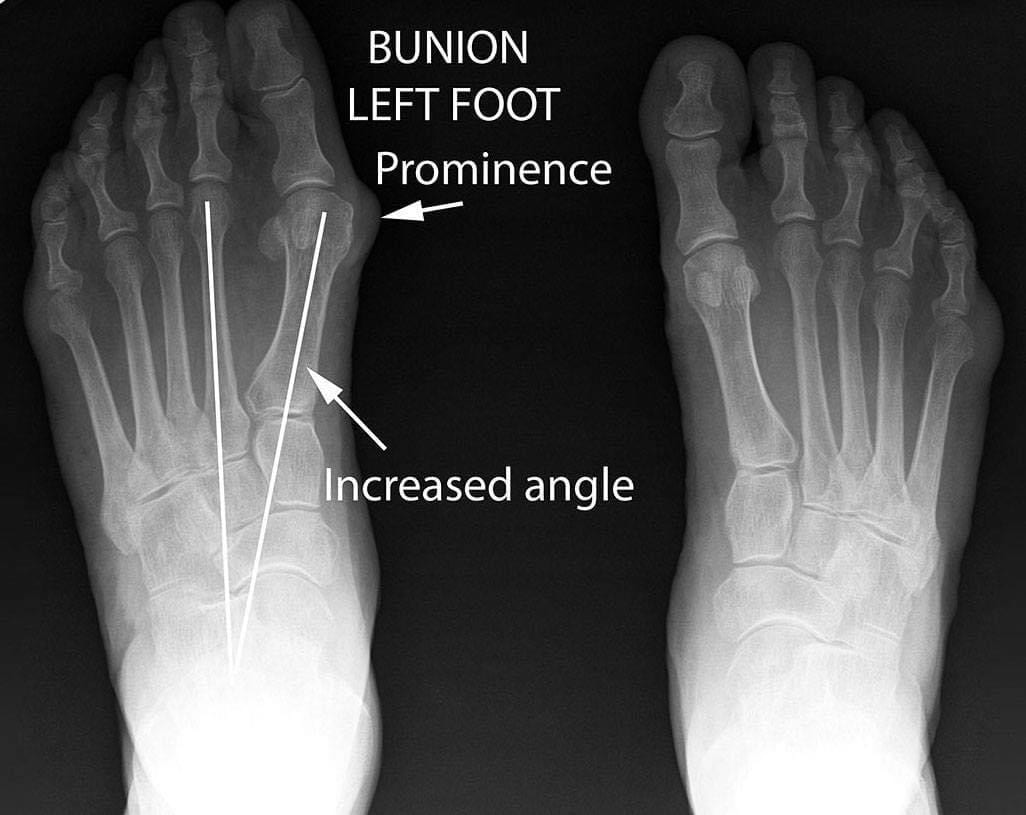
What are Bunions?
A bunion or hallux valgus is a bony deformity affecting the big toe, where there is deviation of the big toe towards the second toe. The first metatarsal joint partially dislocates and often there is a noticeable enlargement or bony prominence around the joint. A poor functioning bunion joint can then lead to arthritic changes within the joint.
Symptoms
Symptoms of bunions can include pain, swelling and inflammation within the metatarsal joint as the joint becomes arthritic. Another source of pain can be rubbing and skin irritation from footwear around the bony prominence. Some bunions can be asymptomatic but this shouldn’t be ignored as bunions generally occur as the result of poor foot function. Bunions can make walking difficult and purchasing good fitting shoes can be a real issue.
Causes
Bunions are primarily caused by poor foot function or excess pronation. Other factors which can cause bunions include genetics (inherited poor foot structure) and poor fitting footwear.
Treatment
Our podiatrists can help relieve bunion symptoms by improving foot mechanics with custom orthotics. If the bunion is treated early then it is often possible to slow down progression of the deformity and help slow down or prevent arthritic destruction of the joint. Bunions that are severe and cause ongoing problems or are unable to fit into the patients preferred footwear may need surgery. In these cases our podiatrists can give you advice and help refer you to a good foot surgeon if required.


What is Foot Arthritis (Hallux Rigidus)?
Hallux rigidus is a term used to describe the condition whereby the joint space in the great toe (hallux) becomes narrowed. This results in reduced range of motion, pain and disability. It is a common condition affecting a large percentage of the community, commonly presents in middle aged women. This is usually attributed to ill-fitting footwear or other co-factors e.g joint mal-alignment.
Diagnosis:
Typically clinical assessment and patient history provides adequate information for diagnosis however often x-ray imaging is utilised to assess the degree of joint space narrowing. Clinical assessments involve assessing the range of motion or amount of movement the great toe is capable of in an upwards and downwards direction before it causes pain and discomfort. Often it is evident the degree of joint space narrowing as range of motion is limited by the bones within the joint rubbing against each other.
Management:
Early intervention is key in preventing hallux rigidus. If excessive pronation, weak muscles and poor footwear are addressed early on our podiatrists are able to reduce the excessive forces applied to the joint and therefore preserve joint space.
Conservative Treatment (early to mid stage):
- Joint mobilisation and manipulation to facilitate motion and reduce inflammation within the joint space
- Footwear – wide, deep shoes with firm sole will aid in reducing bending forces at the impaired joint
- Bespoke modified footwear
- Pharmacological therapy
- Orthotics
- Cortisone injections
Surgical Treatment:
Surgery is often reserved for cases where conservative therapy has either failed or no longer effective due to extent of joint destruction.
In the past results following surgery for hallux rigidus and even bunions had poor outcomes. However, research and implementation of more comprehensive surgical training programs have seen the increase in favourable outcomes following surgery. This involves reduced non-weight bearing times and faster recover with less post-operative complications.
In Australia there are two different methods of addressing hallux rigidus surgically.
Orthopaedic Surgery – Typically involves fusion or immobilisation of the joint
Podiatric Surgery – Involves removing debris/spurs sitting within the joint and preserving joint space by applying new cartilage layer in between the bones of the joint. This maintains the range of motion of the joint therefore improving patient mobility.
Our podiatrists have extensive knowledge on al aspects of surgical intervention for hallux rigidus if you would like further information please do not hesitate to contact us and arrange an appointment to discuss all options.
N.B Our podiatrists are not able to advise on costs of these procedures as they differ greatly depending on the surgeon, hospital and geographical location however they are happy to provide you with the contact information of these surgeons. As with all surgical procedures there are risks associated, please contact your doctor if you are considering surgery to ensure you are a candidate for general/local anaesthetic.
What is Gout?
Gout is a painful inflammation of a joint. The big toe is the joint most commonly affected, although the hands, wrists, knees, ankles, elbows or any other joint can be affected.
Gout is the result of a build of waste material called uric acid, which forms tiny crystals in some of the joints of the body. Uric acid is normally found in the blood of all people, and comes from the breakdown of cells, DNA and from the food and drinks we consume each day.
Uric acid is mostly excreted by the kidneys. Too much uric acid builds up in the blood either because it is not excreted quickly enough or because too much is being produced. This excess can end up in the joints as crystals (called ‘urate’). These crystals can cause sudden and severe inflammation of the joint.
Gout is uncommon in women before the onset of menopause. It is more common in men than in women, and in older people than in younger people, but can affect anyone.
What causes Gout?
Male gender and genetic predisposition are two of the highest risk factors, other causes may include but are not limited to:
- Consumption of crustaceans (prawns and other shellfish), red meats, foods high in acid (e.g. oranges, tomatoes) and dairy products
- Excess consumption of alcohol
- Joint trauma
- Hypertension
- Obesity
- Diabetes
- Kidney disease
- Also more commonly seen in age group above 40 years
Treating Gout
Once Gout has been confirmed by your GP either by routine blood tests and plain film x-rays or through aspiration of joint fluid known as urate assay. A management plan can be implemented this typically involves medications to assist with controlling uric acid levels in the blood, footwear modification, joint mobilisations and also orthotic therapy.
If you are experiencing pain in your big toe joint or other joints in your feet an assessment with one of our highly trained Podiatrists will set you on the right path to optimal foot health.
Book your foot health assessment today!



